For many newly diagnosed with cancer, changes in sexual health throughout and after treatment can go overlooked in favor of more urgent matters. However, sexual health and pleasure can hugely affect quality of life and relationships over time. Knowing what to expect can help patients prepare for their new reality.
Of course, each patient’s experience will surely differ based on cancer type, treatment plan, and many other factors. Here are some of the most common changes patients see in their sexual health after a cancer diagnosis and how to face them.
Physical and Mental Symptoms
Cancers in the pelvic area and the treatments used to target them can physically interfere with sexual activity. Treatments like chemotherapy can cause side effects like erectile dysfunction, loss of libido, and vulvovaginal thinning and dryness. All these symptoms may also pose a challenge for those looking to be intimate.
“It is very common for patients to experience changes in their sensitivity,” says Jennifer Vencill, Ph.D., a Mayo Clinic psychologist. Numbness and neuropathy are both common side effects of surgery that can be disruptive to patients’ ability to reach climax.
Aside from physical barriers, the anxiety surrounding diagnosis and treatment can be exhausting for both patients and their partners. This often leads to decreased arousal. The mental load of cancer and its financial and social implications can be just as harmful to sexual health as the physical symptoms.
How to Support Sexual Health: Patients and Partners
Many excellent resources are available to patients; often, all it takes is asking your care team. Medical treatments provided by sexual health specialists are effective in helping with vulvovaginal dryness, sexual pain, erectile concerns, and many other physical symptoms.
For help addressing the mental effects, mental health providers who specialize in sexual health and sex therapy can be life-changing. Many specialize in oncology care and survivorship as well.
According to a Mayo Clinic Blog Post, Regaining Sexual Health After Cancer Treatment, re-exploring one’s body and sexuality can help patients become acquainted with their new sexual needs and boundaries. “Exploration could mean relearning your body sensations and erogenous zones, something that we refer to as body mapping in the sex therapy world,” says Dr. Vencill, “Or it might be getting comfortable in a body that has drastically changed in how it looks or functions. This might mean exploring sexual aids and things that you perhaps previously hadn’t thought about incorporating into your sex life — whether solo or with a partner.”
With preparation and a mindful approach, patients can expect to again find joy in their sexuality and their new normal.
Did you enjoy this article? Look for more information cancer topics on our blog and join our community of support for cancer patients and their caregivers at OncoPower.
When it comes to protecting our health, our immune system is our trusty shield, defending us against invaders like harmful viruses and bacteria. However, individuals with compromised immune systems, like some cancer patients, face an increased risk of infection. Historically, the neutropenic diet has been prescribed to patients whose immune systems may be compromised as a way to prevent infection from pathogenic, meaning bad or harmful, bacteria found in foods.
What is the neutropenic/low-microbial diet?
The neutropenic diet is a type of diet usually used for individuals with weakened immune systems, or those with an absolute neutrophil count (ANC) below 500. The classic or traditional neutropenic diet eliminates all raw foods like raw fruits and vegetables, raw dairy and cheese; soft cheeses like brie, feta, or farmer’s cheese; deli meats, take-out foods, and fermented foods like yogurt and sauerkraut. These foods are avoided due to their higher potential for pathogenic bacteria that could cause infection in those with compromised immune function.
The evidence for the neutropenic diet:
While the neutropenic diet is still prescribed to patients with impaired immunity, there has been some controversy about whether this diet is necessary. Most of the studies that support the use of the neutropenic diet date back to the 1960s and 1970s. These studies placed leukemia patients in isolated tents with restricted airflow, on sterile diets, and used oral nonabsorbable antibiotics to create an environment aimed at minimizing toxin exposure. Not only is this kind of environment not feasible for the average patient, but the results from these studies indicated that while a protected environment did help to prevent infection in those with compromised immune systems, it was unclear how much the sterilized diet actually contributed to the results of the study independently.
A systematic review published in 2019 examined five randomized controlled trials, including 388 patients who primarily had acute myeloid leukemia, acute lymphoblastic leukemia, or sarcoma. After examining the results from all 5 trials, the review reported that there was no significant difference in infection rate between the neutropenic diet group (53.7%) and the unrestricted diet group (50%). The review concluded that prescribing the neutropenic diet was not associated with a decreased infection rate in neutropenic cancer patients.
When it comes to studying the effectiveness of the neutropenic diet, there are a few issues. The studies often involve only a small number of people, and it’s challenging to figure out which factors are actually causing infections in the participants. Because of these limitations, there isn’t enough evidence to say that the neutropenic diet can effectively prevent infections in people undergoing chemotherapy or with weakened immune systems. Additionally, there is no universal definition of the neutropenic diet across institutions and practitioners, making it difficult to discern which type of neutropenic diet may be affecting infection rates. Furthermore, there has been concern surrounding some very restrictive forms of the diet decreasing patient quality of life and potentially increasing incidences of malnutrition by removing many foods, including foods that have beneficial health effects, such as commercially prepared yogurts and fermented foods that may improve gastrointestinal health.
Because of the lack of evidence to support prescribing the neutropenic diet, many major cancer centers, including Memorial Sloan Kettering and MD Anderson Cancer Center, as well as the Academy of Nutrition and Dietetics, have moved away from recommending a strict neutropenic diet in favor of targeted nutrition education around food safety.
Therefore, it’s crucial to prioritize your safety by following basic food safety guidelines during chemotherapy or when your immune system is weak. This means taking precautions to avoid getting sick from potentially harmful bacteria in food. By being careful about food safety, you can reduce the risk of infections, even if the effectiveness of a classic neutropenic diet is still uncertain.
How to follow safe food practices:
When it comes to food safety, there are four key steps to remember: clean, separate, cook, and chill. By following these practices, you can significantly reduce the risk of foodborne illnesses.
Clean
Before handling or cooking any food, thoroughly wash your hands with soap and water for at least 20 seconds. Also, ensure that the surfaces you use for food preparation are clean and sanitized.
Separate
When shopping for groceries, try to keep raw meats, eggs, fish, and poultry away from your other produce and foods. If you are preparing both meats and ready-to-eat foods and produce, make sure to use a separate cutting board for your meats and your vegetables, bread, and other foods that need to be prepared.
When marinating or defrosting meats and poultry in the refrigerator, make sure to store them on the bottom shelf away from your other foods so any juices from the raw meats do not contaminate your other ready-to-eat foods. Store your raw meats in sealed containers or wrap them tightly to ensure they do not leak in the refrigerator.
One common practice that is actually not food-safe is washing raw chicken. Raw chicken is a ready-to-cook food and does not need to be washed in the sink prior to cooking. Doing so could spread harmful bacteria to your sink area and potentially onto your other foods, which could make you sick. Cooking chicken to the appropriate temperature will kill any bacteria present.
Cook
To ensure food is cooked safely, use a food thermometer to check the internal temperature. Different meats have specific temperature requirements:
Whole cuts of beef, veal, lamb, and pork: 145°F
Fish with fins: 145°F or until the flesh is opaque and flakes easily
Ground meats (beef, pork): 160°F
All poultry (including ground chicken and turkey): 165°F
Leftovers and casseroles: 165°F
If using a microwave, follow recommended cooking and standing times. When reheating cooked foods, use a food thermometer to ensure the internal temperature reaches 165°F.
Chill
Bacteria multiply rapidly in the “Danger Zone” between 40°F and 140°F. When bacteria multiply and divide at a rapid pace, they can make you sick. To prevent this:
- Keep your refrigerator at 40°F or below.
- Refrigerate perishable foods like raw meats, milk, cheese, cut fruit, and leftovers within 2 hours. If exposed to temperatures above 90°F, refrigerate within 1 hour.
- Thaw frozen foods in the refrigerator, in cold water, or in the microwave. Avoid thawing on the counter, as it exposes food to the Danger Zone for an extended period.
By following these simple steps, you can maintain food safety and reduce the risk of foodborne illnesses. For more information and specific questions on food safety, reach out to our registered dietitians at OncoPower.
What is the gut microbiome?
Your gut contains more than 1 trillion microorganisms, including bacteria, viruses, archaea, and eukaryotes that live in your small intestine. These tiny organisms are often thought of as bad, but they actually do a lot of good things for your body. In fact, they have a special relationship with us where we both help each other out. This is called a symbiotic relationship.
Some functions of the gut microbiome include:
- Aiding in digestion and absorption of nutrients
- Preventing the proliferation of “bad” bacteria
- Aiding in metabolism of nutrients
- Synthesis of vitamins such as Vitamin K and certain B vitamins
- Synthesis of serotonin, GABA, and other neurotransmitters that affect mood, memory and cognitive function
- Regulating allergy and immune function
- Many, many others
What is Dysbiosis?
Dysbiosis is a condition where the balance of microorganisms in the gut is disrupted, often caused by various environmental and genetic factors. Additionally, as we age, the likelihood of developing gut dysbiosis increases. This imbalance can lead to negative impacts on overall health, including an increase in inflammation in the body. Inflammation is linked to the formation of various types of cancer, highlighting the importance of maintaining a healthy balance of microorganisms in the gut.
Does Dysbiosis in the Gut Microbiome Affect Cancer Treatment?
A recent review published in Gut suggests that knowing the certain kinds of bacteria we have in our gut might be able to tell us how well cancer treatments will work. For example, higher amounts of the bacteria Faecalibacterium and other Firmicutes, a type of bacteria that helps us digest food, are associated with longer survival in multiple myeloma patients on a certain immune checkpoint inhibitor. However, an increase in Faecalibacterium was also shown to raise the risk of a side effect called colitis, or inflammation of the colon, that occurs in response to some cancer treatments. Alternatively, patients with reduced levels of Akkermansia muciniphila were less likely to respond to anti-PD-1, which is another type of cancer treatment. In contrast, patients who responded well to anti-PD-1 treatment had a higher diversity, meaning more species, of gut bacteria and enriched levels of Ruminococcaceae and Faecalibacterium, which are associated with better immune function in the environment created around a cancer tumor.
Two studies conducted by MD Anderson Cancer Center in 2022 revealed patients who survived longer after treatment with immune checkpoint inhibitors showed unique gut microbiome signatures, or common communities of microbes, compared to those who had shorter survival. While the study initially intended to examine the efficacy of immune checkpoint inhibitor therapy in glioblastoma patients, they also collected stool samples from patients as part of the study before and after treatment. They analyzed the gut microbiome composition and compared the results based on patient survival rates. The analysis revealed that increased numbers of Ruminococcus spp. were related to increased odds of survival and increased levels of Eubacterium spp. increased response to treatment. As a result of this exciting, yet unexpected, discovery, many clinical trials on glioblastoma now routinely collect stool samples from study participants. These findings highlight the importance of the gut microbiome in cancer treatment and may drive research on targeted therapies based on microbiome characteristics in the future.
Although this research is crucial for advancing cancer treatment, the study of the gut microbiome is a relatively recent area of investigation, and more research is needed to fully understand the complex relationship between the microbiome and cancer development and treatment. There are many ongoing clinical trials currently recruiting to uncover the role of the microbiome in cancer treatment (e.g. 1,2). For more information on open trials currently recruiting, sign up for OncoPower, and our team can help match you to a clinical trial, absolutely free!
What You Can Do to Support Your Gut During Treatment
Consume High Fiber and Fermented Foods
Many kinds of cancer therapies can harm the gut lining, making it essential to support your microbiome throughout the treatment process. Consuming a well-balanced diet rich in fiber, fruits, and vegetables can aid in feeding beneficial bacteria and improving microbial diversity in the gut. While cancer treatment might impact your appetite, do your best to consume these foods when you can!
Fiber is important for feeding the beneficial bacteria in the gut microbiome to keep out the bad bacteria, but it also functions to support regular bowel movements, control blood sugar levels, and help maintain a healthy weight. Some high-fiber foods include oats, quinoa, black beans, lentils, chickpeas, broccoli, brussels sprouts, kale, chia seeds, flaxseeds, prunes, and figs. Generally, fiber is considered beneficial for most individuals, including cancer patients. However, there are certain types of cancers and situations in which the amount of fiber recommended may need to be lowered including digestive complications, malnutrition, bowel obstruction or blockage, and after certain surgical procedures. Check with your care team for recommendations on how much fiber to include in your diet during treatment.
Additionally, fermented foods, also known as probiotic foods, are excellent sources of beneficial bacteria and can help replenish your microbiome after a round of antibiotics or during treatments that may harm your gut bacteria. Examples of probiotic foods include yogurt, sauerkraut, kefir, kimchi, kombucha, and tempeh.
While taking on fermented food projects at home is fun, make sure to consume only commercially available fermented foods instead of farmer’s markets or homemade fermented foods while you are going through treatment. This is because it’s important to practice food safety while the immune system is compromised. Without the precise combination of ingredients and careful practice in making fermented food, bad bacteria might outcompete the good bacteria which could lead to illness for immunocompromised individuals.
For patients who are experiencing digestive issues, probiotic foods might make negative symptoms, like nausea and diarrhea, worse. It’s important to assess your individual tolerance for fermented foods and work with a dietitian to assess whether adding these foods to your diet would benefit you.
Overall, fermented foods can be a beneficial component of a healthy diet for cancer patients, but it is essential to assess your personal situation and consult your team of healthcare professionals. Your healthcare team can provide guidance on what is suitable for your specific situation and help you make informed decisions about your diet during cancer treatment.
Should You Take a Probiotic?
Over the past decade, probiotics have become increasingly popular among the general population. Although their benefits and effectiveness are still being studied, research suggests that probiotics may improve the diversity of the microbiome, as well as the efficacy of cancer treatments involving immunotherapy. Despite ongoing research, there is still much to learn about the full range of benefits that probiotics may offer in the oncology space.
One scientific review of clinical trials published by the National Institute of Health found that in cancer patients, probiotics can help reduce the negative side effects of chemotherapy and radiation therapy by improving bacterial diversity in the gut. Probiotics also produce helpful substances that fight against harmful bacteria and block their attachment to the intestinal walls. Some studies have found that probiotics can improve immune responses, reduce infectious complications, and even have positive effects on behavioral and cognitive symptoms in cancer patients. More specifically, one study found a positive link between the strain Bifidobacterium longum 1714 and decreased stress reduction and improved memory. Furthermore, a 2019 review reported on a study that linked oral intake of Lactobacillus helveticus R0052 and Bifidobacterium longum R0175 to a decrease in depression symptoms in individuals with major depressive disorder.
In addition, probiotics have been found to have neuroprotective and cardioprotective effects in both animal models and humans. In rat models, a combination of the strains Bifidobacterium breve, Lactobacillus casei, Lactobacillus bulgaricus, and Lactobacillus acidophilus was linked to a reduction in oxidative stress in a myocardial infarction model.
While exciting research is underway to understand the role of probiotic supplements in improving cancer treatment, many commercially available probiotics are not regulated by the FDA and contain a very limited number of bacteria that may not produce a health-altering response. Talk to your doctor or dietitian before taking any new supplements during treatment and they can help in selecting the most appropriate one for your condition and health goals.
Join the community at OncoPower to speak with our Registered Dietitians who can help you learn more about how gut health can impact your cancer treatment.
Dating back 2,400 years ago to the days of Hippocrates, fasting was proposed as a potential treatment for chronic illnesses. This was based on the idea that along with a fever, loss of appetite during illness may be a natural and beneficial response of the body. In recent years, fasting has gained renewed attention from the medical and scientific communities as a strategy for promoting overall health, longevity, and enhancement of cancer treatment.
Fasting is when you intentionally avoid food and beverages (other than water) or consume very little food for cultural or religious practices. Recent science has shown that fasting may increase longevity, reduce cardiovascular disease risk, promote weight loss, improve inflammatory markers, and improve mental clarity. Furthermore, research on animal models suggests that fasting may help to reduce tumor growth, increase the effectiveness of chemotherapy treatments, and alleviate cancer-related side effects. However, more long-term human studies are needed to confirm these findings.
What’s the difference between fasting and dieting for weight loss?
The easiest way to understand the difference is this:
Most diets focus on telling you what to eat, not when to eat.
A fasting protocol may tell you the time you can eat, but not what you are allowed to eat.
While fasting has been incorporated into many weight loss diets, not all diets involve fasting.
What are the different types of fasting?
Periodic Fasting: This is a 2 to 21 day fasting period that can be used for dietary or religious purposes for holidays like Ramadan and Yom Kippur.
Intermittent Fasting: 24-48 hour fasts with days of regular eating in between. This also includes Alternate Day Fasting where one fasts every other day for 24 hours.
Fasting Mimicking Diet: This is a diet designed to mimic a calorie restricted diet. This entails purchasing meal replacements to eat 5 days a week and is a medically supervised protocol.
Time Restricted Feeding: Prolonged nightly fasts spanning 10-16 hours overnight. For example, if you stop eating at 8 pm, you would consume your first meal between 6 am and 12 pm depending on how long you are fasting.
When is fasting appropriate?
It’s worth noting that fasting is only appropriate for individuals who maintain a healthy BMI and follow a nutrient-dense diet during their eating windows, as fasting may lead to malnutrition and dangerous weight loss, especially for those who have already experienced cancer-related weight loss. Therefore, it is essential to consult with a registered dietitian or your care team before considering fasting as a lifestyle change during cancer treatment. Reach out to one of our registered dietitians at OncoPower to see if fasting might be right for you.
What does the research say?
Overweight and obesity is a risk factor linked to at least 13 cancers including colorectal, ovarian, breast, and pancreatic cancers. The exact mechanisms by which obesity increases cancer risk are not fully understood, but it is thought that several factors may contribute including chronic inflammation, hormonal imbalances, changes in metabolism, immune system dysfunction, and increased oxidative stress. Several studies have suggested that fasting may be beneficial for weight loss and, therefore, may reduce the risk of cancer and cancer recurrence by decreasing these pro-cancerous risk factors.
Additionally, a study conducted out of San Diego examined how prolonged nightly fasting affected cancer recurrence and risk of death from cancer in breast cancer patients. The study found that fasting for 13 hours overnight was associated with a 36% reduction in breast cancer recurrence compared to those who did not fast for longer than 13 hours overnight. However, the results also showed that nightly fasts of less than 13 hours were not significantly associated with a higher risk of death from breast cancer or risk of death from all-cause mortality. This research is promising, but more randomized controlled trial studies are needed to verify the validity of the study findings before these suggestions can be made to everyone.
Chemotherapy can damage DNA in both cancerous and normal cells, leading to uncomfortable side effects such as vomiting, diarrhea, fatigue, and loss of appetite. In a 2018 study, researchers investigated the effects of short-term fasting on quality of life and tolerance to chemotherapy in patients with breast and ovarian cancer. Specifically, the researchers looked at changes in quality of life, fatigue, and tolerance to chemotherapy in response to a 24-hour fast before chemotherapy compared to a non-fasting control group. The fasting group followed a protocol of a 24-hour fast before each chemotherapy session, while the control group followed their usual diet throughout the study period. The results of the study showed that the fasting group had less fatigue, better physical and emotional well-being, and improved tolerance to chemotherapy compared to the control group.
In addition to fasting prior to chemotherapy to help with side effects, the fasting mimicking diet (FMD) may also be a promising strategy for improving the efficacy of chemotherapy and enhancing the immune system’s ability to fight cancer. A study published in 2016 found that a FMD was effective in reducing the growth of tumors and increasing the efficacy of chemotherapy in mice with cancer. The FMD was found to reduce the expression of the protein HO-1, which is known to suppress the immune system and promote tumor growth. In addition, the FMD increased the activity of T cells, a type of immune cell that plays a crucial role in destroying cancer cells. The FMD enhanced the ability of T cells to recognize and eliminate cancer cells, leading to improved tumor clearance.
This exciting preliminary research suggests that periodic fasting may have the potential to improve cancer patients’ comfort levels during and after chemotherapy treatment, as well as enhance the effectiveness of treatments. However, further research on human subjects is necessary to confirm these beneficial effects on cancer survivorship and treatment efficacy. Currently, there are ongoing studies (1,2,) that are actively recruiting participants to evaluate the use of short-term fasting as a means of improving chemotherapy and radiation treatments. For more information on open trials currently recruiting, sign up for OncoPower, and we can help match you to a clinical trial, absolutely free!
Looking to learn more or experience the potential benefits of fasting? Our expert Registered Dietitians at OncoPower can provide you with personalized recommendations tailored to your unique needs and goals. Reach out to us today to explore the potential benefits of fasting and discover how we can support you through treatment and recovery.
Cancer patients often have a lack of appetite or no desire to eat. This can be caused by a number of factors including fatigue, depression, worries about treatment, or gastrointestinal side effects like nausea, vomiting, and diarrhea. Additionally, some cancers can produce hormones that impact how the body experiences hunger and fullness.
What can you do when you have no appetite?
Switch Out Large Meals for Smaller Meals
When you have no appetite, it can be quite difficult to sit down to a large plate of food. Because a large meal can be intimidating, smaller meals or snacks can be a much more manageable option. This can help you ensure you are reaching your nutrition goals but are not feeling discouraged by large plates of food that you leave mostly untouched. Having 6-8 snacks per day can be a much better option than 3 large meals every day. When dealing with a lack of appetite, be sure to take full advantage of moments when you are feeling hungry to maximize eating and nutrition during that time.
Make Your Small Meals and Snacks Well Balanced
Making nutritionally balanced meals and snacks is key to meeting your nutritional needs while keeping food volume at a manageable level. Make sure to include a carbohydrate, protein, fat, fruit, and vegetable at every meal or snack to keep your energy levels stable throughout the day. This could be crackers, cheese, and vegetables; a slice of whole wheat toast with peanut butter and banana slices; or cottage cheese with fruit and a side of carrots.
Add in Extra Fat For Energy
Adding extra fat to your snacks and meals can help you meet your energy goals since fat is the most calorically dense macronutrient. This can be in the form of added butter, cheese, gravy, or sauces. Only a small amount of fat packs a big energy punch!
Make Sure You are Weighing Yourself Weekly
Weigh yourself once a week in the morning after using the bathroom and record the number. If you notice the number is going down for more than 2-3 weeks, make sure to contact your care team.
Appetite issues can be frustrating for cancer patients and concerning for caregivers, but ensuring you are getting enough energy to support your body is crucial during treatment. If you have any questions about helping with appetite, reach out to the registered dietitians at OncoPower for more personalized recommendations and support.
References:
Loss of appetite. Managing Cancer-related Side Effects. https://www.cancer.org/treatment/treatments-and-side-effects/physical-side-effects/eating-problems/poor-appetite.html. Published September 14, 2022. Accessed February 17, 2023.
Sleeping problems are a common side effect for cancer patients due to medication side effects, treatments, and other lifestyle factors that may be hindering the ability to get a restful night’s sleep.
Research shows that sleep helps to regulate blood sugar, prevent brain fog and forgetfulness, reduce stress, improve your mood, and strengthen your immune system. All these benefits of good sleep improve both internal health and day-to-day quality of life.1
What causes sleep problems for cancer patients?
- Both radiation and chemotherapy have been reported to affect sleep patterns.2 Ask your provider if the medications you are using could be contributing to your sleep problems.
- Steroid-based medications can sometimes cause sleep disturbances in cancer patients.
- Medications that impact hormone levels, such as antiestrogens (tamoxifen) and aromatase inhibitors, can cause night sweats and hot flashes.3,4
- Some anti-nausea medications can cause inability to fall asleep. If this occurs, notify your care team to potentially switch out your medications.4
How to Manage Sleep Problems
Wind-Down Plan
The first thing to try when looking to improve sleep is establishing an effective nightly wind-down routine. This can include lifestyle modifications like going to bed at the same time every night, changing the timing of your medications, practicing meditation, controlling the temperature in the room before and during sleep, and turning off all screens 1-2 hours before bed. Establishing a consistent sleep routine is an easy way to prime your body and brain for a good night’s sleep.
Exercise
Exercise has been studied in cancer patients and was shown to help promote sleep and relieve stress.5 This may make you feel more tired at the end of the day to help you fall asleep faster and stay asleep throughout the night. However, it’s important not to engage in vigorous exercises close to bedtime as this can prevent you from being able to fall asleep. Save your hard workouts for earlier in the day and choose more soothing exercises like yoga or stretching for evening movement.
Mindfulness and Meditation
Mindfulness and meditation can be useful relaxation techniques to help you get into a calm state before bed. This can include guided meditation, imagery exercises, calming music, and breathing exercises. Check out OncoPower’s meditation resources or set up an appointment with our meditation specialist.
Nutrition
While you might not think of your eating habits as contributing to sleep disturbances, there are a few eating behaviors you can change to help you fall asleep and stay asleep at night. Try to avoid drinking caffeine post 2 pm or about 6-8 hours before bedtime. Caffeine is a stimulant, which can make you feel alert and prevent you from falling asleep. Additionally, although a sedative, alcohol can also contribute to sleep problems by reducing the amount of time you are in REM sleep, the most mentally restorative part of the sleep cycle. It’s best to avoid alcohol when experiencing trouble sleeping.6
Melatonin is a hormone that controls the body’s sleep-wake cycles. Melatonin production naturally goes down during the day when it’s light out and increases at night when it’s dark to make you tired and get the body ready for sleep. You can try adding natural melatonin-enhancing foods like nuts, oats, tart cherries, and Gogi berries to your meals and snacks to boost your melatonin.7
Medications
If lifestyle modifications are not helping to alleviate your sleep disturbances, some medications may be temporarily used to help with sleep. However, it’s important to consult your care team before taking any medications, supplements, or herbs, including CBD, that claim to help with sleep. This is because they can sometimes cause unwanted drug interactions with cancer medications.
Sleep Apnea
If you are experiencing trouble sleeping, your provider may order a sleep study to assess you for sleep apnea. Sleep apnea is a common sleep disorder in which your breathing may stop or get very shallow while sleeping. These breathing disturbances may cause individuals to feel fatigued the next day despite sleeping for an appropriate amount of time. Consult a doctor or sleep specialist to learn more about making a plan to address your sleep apnea.2
Other Things You Can Do To Manage Sleep-Wake Disturbances
- Keep track of your sleep or wear a fitness tracking device that records your sleep
- Avoid taking naps throughout the day
- Make sure you are following your medication schedule and taking medications at the same time every day. Try OncoPower’s pill reminder feature to help with medication consistency.
- Use blue light-blocking glasses if using screens before bed
- Try to go to bed at the same time every night
Making sleep a priority is essential for overall wellness, but it is especially important after a cancer diagnosis. If you have any questions about sleep, join our community, and be sure to check out the free meditation resources on the OncoPower App.
References
- Physical Health and sleep: How are they connected? Sleep Foundation. https://www.sleepfoundation.org/physical-health. Published April 14, 2022. Accessed March 30, 2023.
- Managing sleep problems. American Cancer Society. https://www.cancer.org/treatment/treatments-and-side-effects/physical-side-effects/sleep-problems/managing-sleep-problems.html. Published January 6, 2020. Accessed February 17, 2023.
- PDQ® Supportive and Palliative Care Editorial Board. PDQ Hot Flashes and Night Sweats. Bethesda, MD: National Cancer Institute. Updated <07/29/2021>. Available at: https://www.cancer.gov/about-cancer/treatment/side-effects/hot-flashes-pdq. Accessed <03/20/2023>. [PMID: 26389162]
- Difficulty sleeping (insomnia). Difficulty sleeping UK. https://www.cancerresearchuk.org/about-cancer/coping/physically/difficulty-sleeping. Published February 14, 2020. Accessed February 17, 2023
- Mustian KM, Sprod LK, Janelsins M, Peppone LJ, Mohile S. Exercise Recommendations for Cancer-Related Fatigue, Cognitive Impairment, Sleep problems, Depression, Pain, Anxiety, and Physical Dysfunction: A Review. Oncol Hematol Rev. 2012;8(2):81-88. doi:10.17925/ohr.2012.08.2.81
- Alcohol and sleep. Sleep Foundation. https://www.sleepfoundation.org/nutrition/alcohol-and-sleep. Published March 17, 2023. Accessed March 30, 2023.
- Melatonin: What you need to know. National Center for Complementary and Integrative Health. https://www.nccih.nih.gov/health/melatonin-what-you-need-to-know. Accessed March 30, 2023.
During Women’s History Month this March, we honor women in the oncology field who have made groundbreaking contributions to the advancement of cancer treatments, research, and care.
In a historically male-dominated field, women in oncology and research have been trailblazing anticancer discoveries for decades. According to a recent survey by the American Society of Clinical Oncology Journal, women make up only 35.8% of the oncology workforce. However, despite this underrepresentation, women’s impact on cancer care will forever be an invaluable part of cancer survivorship today.
5 Women Who Have Made an Impact on Cancer Care
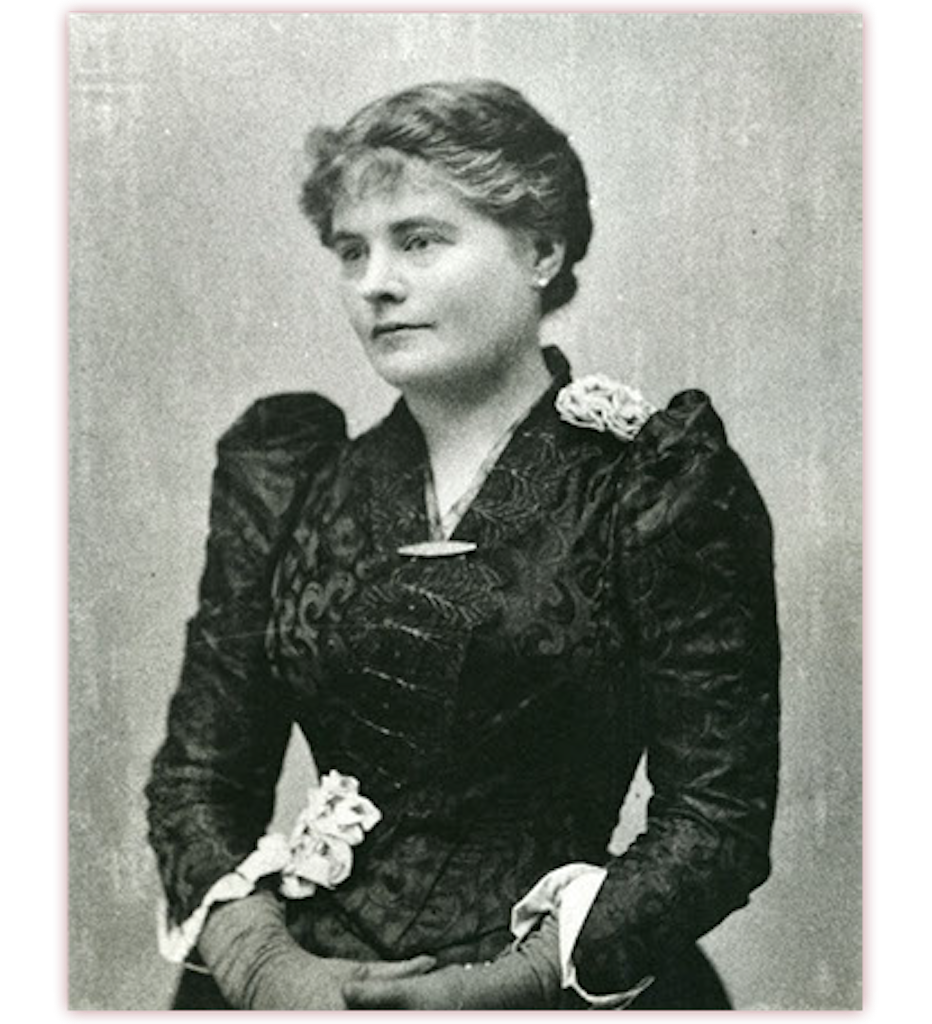
#1 Rose Hawthorne Lathrop
Rose Hawthorne Lathrop was the daughter of American author Nathaniel Hawthorne. In 1896, at the age of 45, she began her nursing education at what is now Memorial Sloan Kettering Hospital, the first US hospital to offer training in cancer care. After completing her nursing education, Hawthorne became one of the first oncology nurses and a trailblazer in terminal cancer care. She dedicated the second half of her career to helping cancer patients in poverty, as cancer was a misunderstood and stigmatized disease in the 19th century that some believed was contagious and due to poor hygiene.1,2,3

#2 Jane Cooke Wright, MD
Jane Cooke Wright was a surgeon and cancer researcher who pioneered research in clinical chemotherapy agents for cancer treatment. Together with her father, Louis Wright, who founded the Cancer Research Center at Harlem Hospital, they began experimenting with chemical agents on mice with leukemia. Wright and her father began treating patients with their anticancer agents and found many experienced some form of remission. Wright continued to research chemotherapeutic agents for cancer treatment throughout her career and developed several techniques for chemotherapy administration. She also received the recognition of being the highest-ranked Black woman at an American medical institution and was appointed as a professor of surgery, head of the chemotherapy department, and associate dean at New York Medical College in 1967. Wright was also the first woman elected president of the New York Cancer Society. 1,4
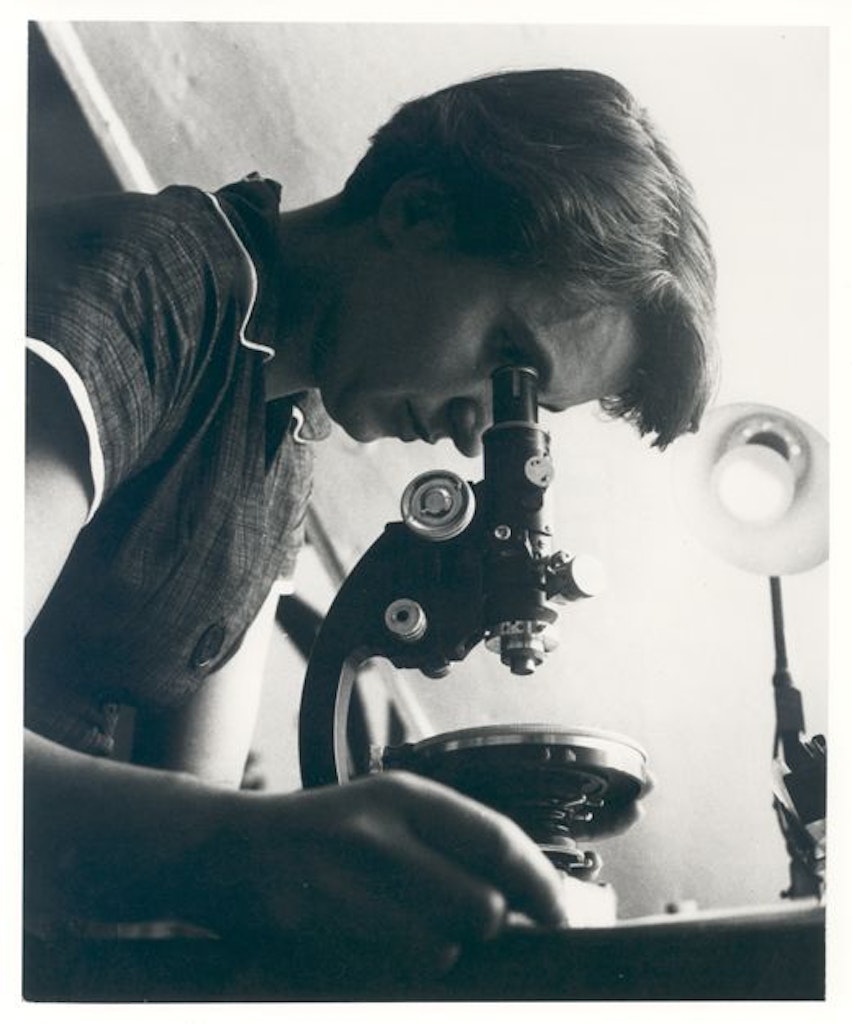
#3 Rosalind Franklin
Rosalind Franklin was a chemist from the UK whose discoveries greatly influenced the scientific community’s understanding of DNA and RNA. In the 1950s, Franklin was working in a lab with x-ray diffraction images of large biological molecules, which led to the discovery of the DNA double helix via a photo taken by her graduate student, Raymond Gosling. In 1962, the Nobel prize was awarded to James Watson and Maurice Wilkins for this discovery. Part of her work in x-ray diffraction led to her brilliant discovery of a humidity-controlled camera chamber, which allowed the x-ray to produce clearer images. Cancer research today relies heavily on pinpointing the genetic origins of cancer using DNA and RNA, which would not have been possible without Franklin’s discovery in the 1950s. 1,5,6

#4 Angela H. Brodie, Ph.D., FAACR
Angela H. Brodie was a scientist whose research led to the discovery of therapies used to treat breast cancer. Brodie was a distinguished professor at the University of Maryland School of Medicine and was a key player in the development of the first selective aromatase inhibitor, which can prevent the growth and spread of breast cancer. While her discovery was initially met with some skepticism, this breakthrough is considered one of the most influential and important discoveries in treating estrogen-driven breast cancers.7

#5 Edith H. Quimby, ScD
Edith H. Quimby was a physicist who pioneered the use of therapeutic x-rays and radium. She focused mainly on the effects of radiation and how to adjust the dosage to produce the fewest side effects for patients. In the radiology field, she is known for her “Quimby Rules”, a set of guidelines used by radiation oncologists to determine the specific placement of radium needles during cancer treatments. Quimby received numerous honors and awards throughout her life and co-authored the first physics textbook for radiologists: “Physical Foundations of Radiology”.8

BONUS #6 Mary-Claire King, Ph.D.
Mary-Claire King is a geneticist and a professor at the University of Washington, Seattle. King is best known for her discovery of the BRCA1 gene mutation or the “breast cancer gene” that linked some breast cancer with genetics. This discovery revolutionized cancer care by allowing those with the BRCA1 genetic mutation to get screened earlier and more often to detect cancer prior to advanced-stage development. In 2016, King was awarded the National Medal of Science for her work with the BRCA1 gene and her humanitarian efforts in which she used PCR gene sequencing to help identify and reunite more than 100 Argentinian children with their biological families. King also contributed to new discoveries in forensics by harvesting mitochondrial DNA from teeth to identify the remains of soldiers from the Vietnam War, Korean War, and WWII.9,10
OncoPower is a proud female-founded company that celebrates amplifying women’s voices in the medical field and beyond. Join our community of patients and professionals today and access information on nutrition, mindfulness, managing side effects, and view Q&A sessions with oncology experts.
Sources:
- https://www.cancersupportcommunity.org/blog/5-women-who-helped-shape-cancer-care
- https://voice.ons.org/news-and-views/celebrate-pioneers-across-oncology-this-womens-history-month
- https://www.workingnurse.com/articles/rose-hawthorne-lathrop-1851-1926/
- https://www.aacr.org/professionals/membership/aacr-academy/fellows/jane-cooke-wright-md/
- https://www.wikiwand.com/en/Rosalind_Franklin
- https://profiles.nlm.nih.gov/spotlight/kr/feature/biographical
- https://www.aacr.org/professionals/membership/aacr-academy/fellows/angela-h-brodie-phd/
- https://www.miragenews.com/womens-history-month-women-at-cuimc-who-made-735663
- https://www.jax.org/news-and-insights/jax-blog/2017/february/mary-claire-king
- https://www.bcrf.org/researchers/mary-claire-king
Our Mind’s Are Always Racing
In our day to day lives, our minds tend to be always ‘on’. We are constantly replaying stories in our head of what’s to come and what’s going to happen to us in the future. Or we find ourselves in a spiral of rehashing conversations and situations from past events, whether they happened one day or 20 years ago.
Does this sound familiar?
Tuning Into The Present Moment
Stress and anxiety occurs when we are living either in the past or in the future. The present moment is all we ever have, yet we are never really being ‘present’ in our day to day lives. Instead we are worrying, overanalyzing, contemplating, and stressing over situations and events that are either long gone or haven’t even happened.
This is especially true if you receive a cancer diagnosis. A cancer diagnosis can immediately spring your thoughts into a false ‘story’ of future events that hasn’t even happened yet, or perhaps is not going to happen at all. We take ourselves out of the present moment or the ‘now’ and spring ourselves into a fearful story that our mind begins to weave and make up.
This is why it’s so important to have a meditation practice to bring your thoughts and awareness back to the present. And to also view the stories simply as what they are – just stories.
Meditation And Living In The Present
Meditation has assisted many cancer patients with restoring a feeling of calm by centering their thoughts, all while dissipating fears about the future and regrets about the past.
When you meditate, you learn how to become fully present in the here and the now. Meditation expands your senses and deepens your connection to life. It takes you out of living in the ‘past’ or ‘future’. You begin to learn how to be more open to the fullness and beauty in every single moment, even if you are going through cancer treatment. This alone helps free your mind from thoughts that can overwhelm or consume you.
Meditation expands your awareness beyond thought. You start to become aware of what is present in the moment without getting caught up in your thoughts. Meditation brings awareness without adding thought. You become more present and notice more sights, sounds, and sensations. Your connection to life is renewed. Meditation is not about stopping thoughts, but not stopping at them. We are human, thoughts will always arise. Thoughts are just something to observe, not get rid off. Anxiety, stress, and grief occurs when we identify with a particular thought.
Practices to live in the Present Moment:
• Mindful Walking
• Art
• Yoga
• Body Scan
• Morning Pages/Journaling
• Visualizing Daily Goals
• Boxed Breathing
Additional Techniques:
• Pay attention to your breathing. Take a few moments throughout the day to focus on your inhales and exhales.
• During times of stress. Pause. Take a breather, a few moments to yourself in silence.
• Choose an activity during the day where you can practice Mindfulness. Doing the dishes, brushing your teeth, walking from your car to your office. Pay attention to each movement and sensation, not letting your mind wander off.
Begin Your Meditation Journey With OncoPower
If you are unsure how to kickstart your mindfulness journey, make sure to visit our OncoPower app to access our meditations for oncologists and meditations for cancer healing and cancer supoprt. Here you can also find additional resources and access to a large community of oncologists and cancer patients.
And if you are interested in a 1:1 consultation with a Meditation teacher, make sure to book a free consultationwith Natalie Thomas, our dedicated Meditation cancer care and oncologist specialist at OncoPower, who can assist you on your mindfulness journey. Utilize our cancer support services today.
The End of A Chapter
As we inch closer to the holiday’s and the end of December, it’s pretty hard to believe that 2022 is about to come to an end. For many, this proved to be a challenging year, as we integrated back into the ‘new normal’ after Covid, dealt with the rising demands in our day to day lives, and/or have been going through cancer treatment.
Celebrate The ‘Wins’ of 2022
While December can be a stressful time, it’s also a time for a personal celebration. It’s t time to reflect back on this year and to celebrate the small wins of 2022. Many times we put so much pressure on ourselves that we neglect the ‘small’ or ‘big’ moments of accomplishment and happiness in our lives. It can be as simple as feeling more at peace in your life. It’s through stepping into a state of gratitude where we are able to realign our energy and give thanks to where we are at, no matter what happened in 2022.
Mindfulness Tools & The New Year
As a mindfulness teacher and coach, it is so important to focus on a wellness routine as you enter into the new year, and a new chapter. Mindfulness practices assist you in releasing stress and anxiety that cancer can bring, healing your physical body, helping you live more in the present moment, improving sleep, and aiding in decreasing depression.
Instead of making new year’s resolutions, I encourage you to focus on meditation and your mindfulness tools. It’s through the practice of going inwards where you begin to shift your outer reality and move closer towards your goals. By cultivating a wellness routine, it’s scientifically proven that you will heal faster, both physically and emotionally.
Benefits of a Wellness Routine
Even by taking just five minutes a day to sit in silence, taking a walk outside, or practicing controlled breathing, you will start to embark on your mindfulness journey. Meditation especially will guide you into a deeper understanding of yourself and the environment around you. Meditation will assist you in calming the thoughts running through your mind, as you begin to cultivate a new found sense of awareness. Your relationships will change, your outer environment will change, and most importantly, YOU will change, all for the better.
Meditation Resources
If you are unsure where to begin as you enter 2023, OncoPower has some excellent resources to assist you in kickstarting your meditation practice. I am also available for 1:1 meditation sessions where you will practice breathing techniques, light stretches, and guided meditations to help you decrease stress, anxiety, and depression that cancer can bring. Whether you are a seasoned meditator or have never meditated before, our 1:1 sessions together are for all levels. You can book a meditation consultation with me using the link HERE.
Tools & Tips:
Below are also some helpful tools and tips that you can cultivate in your day to day life as you enter into a new year. By just setting the intention of practicing mindfulness, you have already embarked on your journey.
Mindfulness Practices For 2023:
- Boxed Breathing (see our Meditation Suite at OncoPower)
- Walks in nature
- Meditating
- Journaling
- Expressing gratitude
- Light stretches
- Setting a daily intention when you wake up
- Drawing or creating art
- Take a bath with epsom salt
- Practice Yoga
- Get at least eight hours of sleep
- Laugh with others
- Take a digital detox
- Declutter your home
Just by taking 10-15 minutes a day to practice mindfulness, you begin to fill your own cup. Refer back to the check-list and see which practices resonate most with you. All practices will help you while you go through cancer treatment.
Please know you are not alone and it is never too late for change. At OncoPower, we are here to assist you every step of the way.
“The process of healing begins when we mindfully breathe in.” – Thich Nhat Hahn
What Is Mindfulness?
Mindfulness in simple terms refers to the quality or state of being conscious or aware of something.
Mindfulness is an overall mental state that is achieved by focusing one’s awareness on the present moment – away from the past and the future. Mindfulness has to do with acknowledging and accepting one’s thoughts, feelings and bodily sensations without judgment.
Mindfulness Practices
There are many forms of mindfulness practices such as meditation, breathing exercises, visualizations, journaling, sensory exercises, creativity (to name a few). By practicing mindfulness techniques you begin to focus on being intensely aware of what you’re sensing and feeling in the moment, without interpretation.
In fact, mindfulness practices serve as highly therapeutic and beneficial to one’s mental, physical, and emotional state, especially when going through your cancer journey.
Through the practice of mindfulness, you begin to fully relax the body and mind, in term helping you reduce stress. Mindfulness techniques are a great tool to use to help you cope with cancer treatment and a cancer diagnosis.
Why Practice Mindfulness?
Mindfulness can assist you with regaining your overall help. It helps you to become fully present in the moment, aware of where you are and where you are going. Many times we are operating on autopilot – and fear. Fear keeps us in a negative mental state, which can lead to increased anxiety and depression. Mindfulness exercises take us out of this emotional hijack to better cope with life’s stresses, such as cancer.
Mindfulness and Cancer
It is said that mindfulness practices for cancer can create better outcomes for patients by helping them focus on the present moment, taking them away from the worry of the unknown that cancer brings.
Stress and anxiety occurs when you are thinking of what has happened to you in the past, and/or what is going to happen in the future. Constantly thinking and worrying about your cancer diagnosis can lead to increased stress, depression, and deterioration of overall health.
By practicing mindfulness for cancer patients, you begin to not think about what is going to happen in the past or the future. And instead, can observe what is happening right here and right now in this moment.
Connecting Back To Yourself
Mindfulness for cancer patients can assist you in connecting within yourself – back to who you truly are. Many times we can abandon ourselves and forget to take care of our basic needs.
We tend to put others before ourselves, which can leave us feeling drained. It is very important to fill your own cup first before others. We cannot give to others which we do not have ourselves.
Through mindfulness practices, you begin to fill your own cup and self worth, even while going through cancer treatment. Just taking a few moments to yourself to practice meditation and to mindfully breathe, you begin to connect back to YOU. Your cup becomes more full and life tends to become more positive and bright.
Taking a moment to pause to practice mindfulness for just a few minutes at different times throughout the day can help you feel much better, and heal much faster, from cancer.
Benefits of Practicing Mindfulness:
- Reduces stress, anxiety, and depression
- Improves sleep
- Reduces chronic pain
- Improves concentration
- Assists with weight loss
- Restores emotional balance
- Increases resiliency
How to Practice Mindfulness:
- Take three deep breaths
- Practice Meditation and/or Yoga
- Give gratitude
- Observe your thoughts and feelings
- Take a mindful walk
- Journaling
To kick start your mindfulness journey, make sure to check out the OncoPower App for guided meditations, affirmations, and deep breathing exercises.
On the app you can also find cancer care specialists, treatment recommendations, and a cancer support community.
Our Mindfulness coach and Meditation teacher, Natalie Thomas, is also available for 1:1 support. CLICK HERE to sign up for your free meditation class with Natalie.